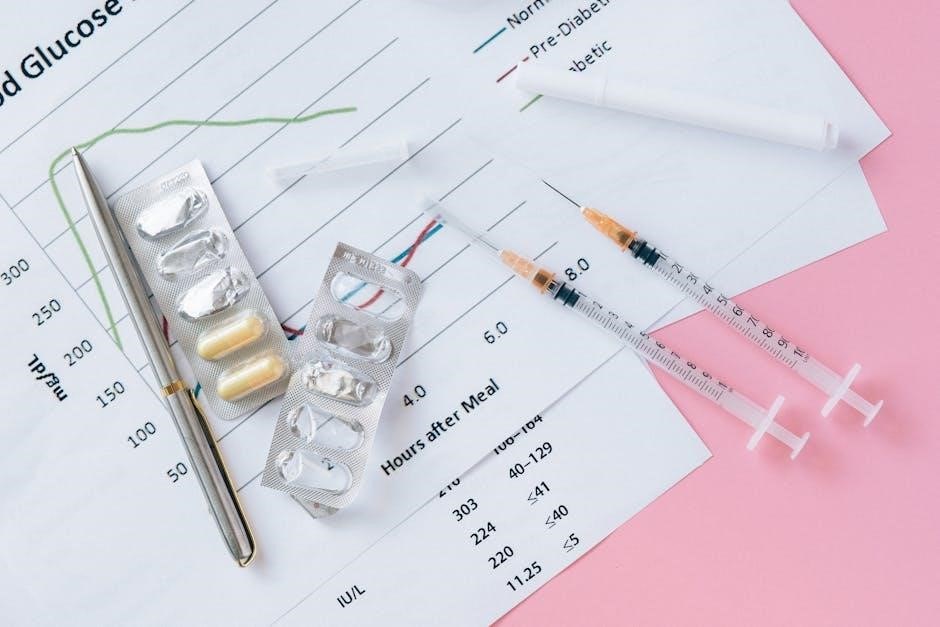
A sliding scale insulin chart is a tool used to adjust insulin doses based on blood sugar levels, helping manage diabetes effectively. It’s personalized for individual needs.
What is a Sliding Scale Insulin Chart?
A sliding scale insulin chart is a personalized tool used to determine insulin doses based on blood sugar levels. It provides a structured approach to adjusting insulin amounts, helping individuals with diabetes maintain blood sugar control. Typically created by healthcare providers, the chart outlines specific insulin doses for different blood glucose ranges, allowing for tailored management. It is a flexible method that adapts to varying blood sugar levels throughout the day, supporting effective diabetes care.
Importance of Sliding Scale Insulin Charts in Diabetes Management
Sliding scale insulin charts play a crucial role in diabetes management by enabling precise and timely insulin adjustments. They help maintain blood sugar levels within a healthy range, reducing the risk of complications. These charts are particularly useful for individuals with fluctuating glucose levels, offering a flexible approach to insulin therapy. By tailoring doses to specific blood glucose readings, they promote better glycemic control and enhance overall diabetes care, making them a valuable tool for both patients and healthcare providers.

How Sliding Scale Insulin Charts Work
Sliding scale insulin charts adjust insulin doses based on blood sugar levels, providing a structured approach to manage glucose fluctuations effectively for patients with diabetes.
Blood Sugar Levels and Corresponding Insulin Doses
A sliding scale insulin chart maps blood sugar levels to specific insulin doses, ensuring personalized treatment. For example, a blood sugar range of 70-130 mg/dL may require 0 units, while levels above 250 mg/dL might need 15 units or more. The chart provides a clear, structured approach to insulin administration, helping patients and healthcare providers manage glucose fluctuations effectively and maintain target blood sugar levels throughout the day.
Adjusting Insulin Dosage Based on Blood Glucose Readings
Adjusting insulin dosage based on blood glucose readings is a core feature of sliding scale insulin charts. Higher blood sugar levels trigger increased insulin doses, while lower levels may require no additional insulin. This structured approach ensures personalized treatment, allowing for precise adjustments to maintain target blood sugar levels. By tailoring insulin doses to individual glucose readings, the chart helps prevent hyperglycemia and hypoglycemia, promoting better diabetes control and reducing long-term complications.

Components of a Sliding Scale Insulin Chart
A sliding scale insulin chart includes blood sugar ranges, corresponding insulin doses, and meal-related adjustments, providing a structured framework for personalized diabetes management.
Blood Sugar Ranges and Insulin Dosage Columns
The chart includes columns for blood sugar ranges and corresponding insulin doses. Ranges like 70-130, 131-150, and 151-200 are paired with specific insulin units, such as 0, 3, or 5 units. This structured format helps users quickly determine the appropriate dose based on their glucose levels. The columns are organized to provide clear guidance, ensuring accurate insulin administration and effective blood sugar management. This setup is essential for personalized diabetes care and maintaining target glucose levels.
Meal-Related Insulin Adjustments
Meal-related insulin adjustments are integrated into sliding scale charts to account for blood sugar fluctuations after eating. Insulin doses are calculated based on pre-meal blood glucose levels, with higher readings requiring more units. For example, a blood sugar of 151-200 might require 4 units, while 201-250 necessitates 6 units. This approach ensures personalized dosing, improving post-meal glucose control and reducing variability. It’s particularly useful for individuals with varying meal schedules or carbohydrate intake, promoting precise blood sugar management.

Types of Sliding Scale Insulin Charts
Sliding scale insulin charts are categorized into low-dose, medium-dose, and high-dose scales, tailored to individual insulin sensitivity and blood sugar management needs.
Low-Dose Sliding Scale
The low-dose sliding scale is designed for individuals with lower insulin needs, often elderly or thin patients. It starts with minimal insulin doses, adjusting gradually as blood sugar levels rise. This approach minimizes hypoglycemia risks while maintaining blood sugar control. For instance, a blood sugar level of 71-119 mg/dL requires no additional insulin, while levels above 150 mg/dL may need 2-3 units. This scale is typically used under medical supervision to ensure safety and effectiveness.
Medium-Dose Sliding Scale
The medium-dose sliding scale is suitable for patients with moderate insulin requirements. It typically starts with a baseline dose, adjusting based on blood sugar levels. For example, levels below 70 mg/dL are treated for hypoglycemia, while levels between 120-150 mg/dL require 2 units of insulin, increasing to 4 units for 151-200 mg/dL, and 6 units for 201-250 mg/dL. This scale balances glucose control and minimizes hypoglycemia risks, making it ideal for patients with stable blood glucose patterns.
High-Dose Sliding Scale
The high-dose sliding scale is designed for patients with significant insulin resistance or those requiring larger insulin doses; It starts with higher baseline doses and escalates rapidly. For instance, blood sugar levels above 250 mg/dL may require 15 units of insulin, with further adjustments as needed. This scale is often used in critical care settings or for patients with severe hyperglycemia, ensuring rapid glucose control while closely monitoring for hypoglycemia risks.

Benefits of Using a Sliding Scale Insulin Chart
- Improved blood sugar control through personalized dosing.
- Reduces hypoglycemia risk by tailoring insulin to glucose levels.
- Offers flexibility for patients with varying insulin needs.
Improved Blood Sugar Control
A sliding scale insulin chart enhances blood sugar management by tailoring insulin doses to specific glucose levels, reducing variability. This approach helps maintain target ranges, preventing extreme highs or lows. By adjusting insulin based on real-time readings, it minimizes hyperglycemia and hypoglycemia risks. Consistent use can lead to better long-term glucose control, lowering the risk of diabetes-related complications. It’s a practical solution for individuals requiring precise insulin adjustments to stabilize their blood sugar levels effectively.
Reduced Risk of Hypoglycemia
The sliding scale insulin chart minimizes hypoglycemia by adjusting doses according to blood sugar levels, ensuring insulin administration aligns with current needs. This method prevents excessive insulin delivery when glucose is low, safeguarding against dangerous drops. By customizing doses, it reduces the likelihood of severe hypoglycemic episodes, enhancing patient safety and overall well-being. Regular monitoring and tailored adjustments further mitigate risks, making it a reliable strategy for managing diabetes with reduced hypoglycemia concerns.
Flexibility for Different Patients
Sliding scale insulin charts offer flexibility, catering to diverse patient needs. They accommodate variations in age, weight, and insulin sensitivity, allowing personalized adjustments. This adaptability ensures tailored insulin doses for different lifestyles and health conditions, making it suitable for both type 1 and type 2 diabetes. By adjusting doses based on blood sugar levels, the chart provides a customizable approach, enhancing its effectiveness for a wide range of individuals with unique diabetes management requirements.

Creating a Personalized Sliding Scale Insulin Chart
Creating a personalized sliding scale insulin chart involves assessing individual factors like age, weight, and insulin sensitivity. Healthcare providers develop tailored charts, considering blood sugar levels, diet, and activity. The chart is adjusted based on insulin requirements, with regular monitoring to ensure effectiveness and safety. It requires continuous collaboration between patients and providers to manage diabetes successfully.
Steps to Develop a Custom Chart
Assess individual factors such as age, weight, and insulin sensitivity to determine insulin needs.
Set up blood sugar ranges with corresponding insulin doses in consultation with a healthcare provider.
Adjust the chart based on diet, activity levels, and lifestyle changes to ensure flexibility.
Regularly monitor blood sugar levels and insulin doses, updating the chart as necessary.
Present the information clearly, possibly in a digital or printed format.
Choose between low-dose, medium-dose, or high-dose scales based on individual needs.
Educate the individual on proper chart usage, including how to read it and adjust doses.
This collaborative process ensures the chart is effective and tailored to the person’s specific requirements.
Factors to Consider (Age, Weight, Insulin Sensitivity)
Age, weight, and insulin sensitivity are crucial factors when developing a sliding scale insulin chart. Younger individuals may require different doses than the elderly. Weight influences insulin dosage, as larger body mass often needs higher doses. Insulin sensitivity varies among individuals, with some requiring less insulin due to better glucose uptake. These factors ensure personalized and effective blood sugar management, tailored to the individual’s unique physiological needs.

How to Use a Sliding Scale Insulin Chart in Practice
Check blood sugar levels before meals and at bedtime. Use the chart to find the corresponding insulin dose based on current readings and administer as directed.
Practical Application for Patients
Patients use sliding scale insulin charts to adjust doses based on blood sugar levels, typically before meals and at bedtime. They match their blood glucose reading to the chart’s range, then administer the corresponding insulin units; This method allows for flexibility, as doses can vary daily based on glucose fluctuations. Patients should consistently monitor their levels and consult their healthcare provider for adjustments. The chart simplifies insulin management, helping patients maintain better blood sugar control and reduce hypoglycemia risks.
Monitoring and Adjusting the Chart
Regular monitoring of blood sugar levels is essential to ensure the sliding scale insulin chart remains effective. Healthcare providers track blood sugar trends to assess insulin dose accuracy. If blood sugar levels consistently fall outside target ranges, the chart may need adjustments, such as modifying insulin-to-carbohydrate ratios or correction factors. Patients should collaborate with their healthcare team to fine-tune the chart, ensuring optimal blood sugar control and minimizing risks like hypoglycemia. Adjustments are typically made based on individual responses and lifestyle factors.
Sliding Scale Insulin Chart vs. Other Insulin Management Methods
A sliding scale insulin chart offers personalized, flexible dosing based on blood sugar levels, unlike fixed-dose regimens or insulin pumps, making it adaptable for varying glucose patterns.
Comparison with Fixed-Dose Insulin Regimens
A sliding scale insulin chart differs from fixed-dose regimens by adjusting insulin doses based on real-time blood sugar levels. Fixed-dose plans use consistent amounts regardless of glucose readings, potentially leading to less precise control. The sliding scale offers flexibility, allowing patients to adapt their insulin intake to daily fluctuations, while fixed-dose regimens may be simpler but less responsive to changing needs. This adaptability makes sliding scale charts more effective for managing variable blood sugar patterns.
Advantages Over Insulin Pumps
A sliding scale insulin chart offers simplicity and cost-effectiveness compared to insulin pumps. It eliminates the need for complex device management, making it more accessible for patients. Unlike pumps, sliding scale charts provide a straightforward method for insulin dosing adjustments, reducing the risk of technical errors. This approach is ideal for patients who prefer a less invasive and easier-to-use system, offering flexibility without the burden of continuous device monitoring and maintenance;

Safety Considerations and Potential Drawbacks
The sliding scale insulin chart carries risks of over-insulinization, potentially causing hypoglycemia. Regular blood sugar monitoring is crucial to avoid dangerous drops in glucose levels and ensure safe usage.
Risks of Over-Insulinization
Over-insulinization can lead to hypoglycemia, a dangerous condition with symptoms like dizziness, confusion, and loss of consciousness. Severe cases may require medical intervention. Regular blood sugar monitoring is essential to prevent this risk. Patients must adhere to prescribed dosage guidelines to avoid overcorrection of glucose levels. Healthcare providers should closely monitor individuals using sliding scale insulin charts to minimize these risks and ensure safe insulin management practices.
Importance of Regular Blood Sugar Monitoring
Regular blood sugar monitoring is crucial for maintaining tight glucose control and preventing complications. It helps identify trends and patterns, guiding insulin adjustments to avoid hyperglycemia and hypoglycemia. Monitoring ensures the sliding scale insulin chart is used effectively, allowing timely corrections. Consistent checks with a glucometer and logging results in a diabetes journal or app provide valuable insights for healthcare providers to optimize treatment plans and improve overall diabetes management.
Sliding scale insulin charts are an effective tool for managing blood sugar levels, offering flexibility and precision in diabetes care, making them a valuable resource for patients and healthcare providers.
Final Thoughts on the Effectiveness of Sliding Scale Insulin Charts
Sliding scale insulin charts are a practical and adaptable approach to diabetes management, offering precise insulin adjustments based on blood glucose levels. They allow for tailored care, reducing the risk of hypoglycemia and hyperglycemia. While they require regular monitoring and medical guidance, these charts remain a cornerstone in diabetes treatment, especially for those requiring insulin therapy. Their effectiveness lies in their ability to balance flexibility with structured care, making them indispensable for many patients.